Pulmonary Hypertension:
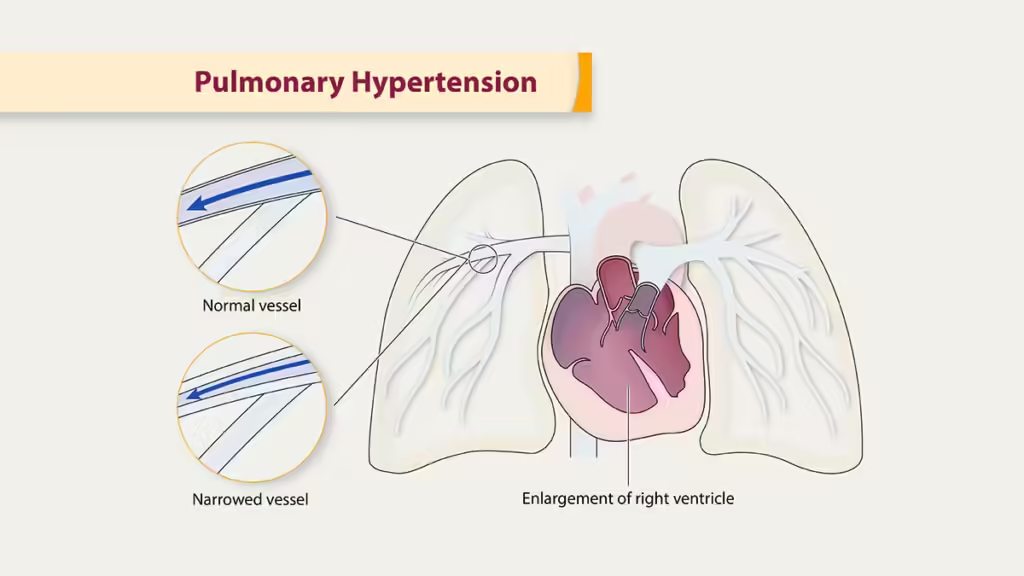
Pulmonary Hypertension (PH) is a type of high blood pressure that affects the arteries in the lungs and the right side of the heart. It occurs when the blood vessels in the lungs become narrowed, blocked, or destroyed, leading to increased pressure in the pulmonary arteries. This makes the right side of the heart work harder to pump blood through the lungs, eventually leading to heart failure if left untreated. PH can be a serious, progressive condition, but early diagnosis and treatment can improve quality of life and outcomes.
Types of Pulmonary Hypertension:
Pulmonary Arterial Hypertension (PAH):
- Description: A type of PH where the small arteries in the lungs become narrowed, thickened, or stiffened, raising the pressure in the lungs. It may be idiopathic (no known cause) or secondary to other conditions.
- Causes: Genetic factors, connective tissue diseases (e.g., scleroderma), congenital heart defects, and certain drugs or toxins.
- Symptoms: Shortness of breath, fatigue, chest pain, dizziness, and swelling in the legs or abdomen.
- Treatment Options: Medications (prostacyclins, endothelin receptor antagonists, PDE-5 inhibitors), oxygen therapy, and in some cases, lung transplantation.
Pulmonary Hypertension due to Left Heart Disease:
- Description: This type of PH is caused by conditions that affect the left side of the heart, such as heart failure, mitral valve disease, or aortic valve disease. The pressure builds up in the lungs as a result of left heart dysfunction.
- Causes: Left-sided heart disease, including heart failure with preserved or reduced ejection fraction, and valvular heart disease.
- Symptoms: Similar to PAH, including shortness of breath, fatigue, and swelling.
- Treatment Options: Managing the underlying heart condition, diuretics to reduce fluid retention, and sometimes medications for heart failure.
Pulmonary Hypertension due to Lung Disease or Hypoxia:
- Description: PH that occurs as a result of lung diseases, such as chronic obstructive pulmonary disease (COPD), interstitial lung disease, or sleep apnea. These conditions lead to low oxygen levels, which cause pulmonary arteries to narrow.
- Causes: COPD, emphysema, interstitial lung disease, sleep apnea, chronic exposure to high altitudes.
- Symptoms: Shortness of breath, fatigue, and a worsening of underlying lung symptoms.
- Treatment Options: Treating the underlying lung disease, oxygen therapy, and pulmonary rehabilitation.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
- Description: CTEPH is caused by chronic blood clots in the lungs that obstruct blood flow and raise pressure in the pulmonary arteries. It is a potentially curable form of PH if treated early.
- Causes: Previous pulmonary embolisms (blood clots in the lungs) that have not resolved properly.
- Symptoms: Shortness of breath, chest pain, palpitations, and leg swelling.
- Treatment Options: Blood thinners, pulmonary endarterectomy (surgical removal of clots), and balloon pulmonary angioplasty.
Pulmonary Hypertension with Unclear Multifactorial Mechanisms:
- Description: This group includes cases of PH with complex or unclear causes, such as blood disorders (e.g., sickle cell disease), metabolic disorders, or systemic conditions that affect multiple organs.
- Causes: Diseases like sarcoidosis, sickle cell anemia, or metabolic disorders.
- Symptoms: Variable, depending on the underlying condition, but may include shortness of breath, fatigue, and chest pain.
- Treatment Options: Depends on the underlying condition, with a combination of therapies targeting the specific cause of PH.
Causes and Risk Factors:
- Genetics: Inherited mutations, particularly in the BMPR2 gene, can increase the risk of PAH.
- Heart Disease: Left-sided heart disease or heart failure can lead to PH.
- Lung Diseases: Chronic lung conditions, such as COPD or interstitial lung disease, are common causes.
- Blood Clots: Chronic blood clots in the lungs can cause CTEPH.
- Connective Tissue Diseases: Conditions such as scleroderma or lupus can affect the lungs and cause PH.
- Sleep Apnea: Untreated sleep apnea can lead to pulmonary hypertension.
- High Altitude: Long-term exposure to high altitudes can lead to PH due to low oxygen levels.
- Drug and Toxin Exposure: Certain appetite suppressants, recreational drugs like cocaine, and chemotherapy agents can increase the risk of developing PH.
Symptoms of Pulmonary Hypertension:
- Shortness of Breath: Especially during physical activity or even at rest in advanced stages.
- Fatigue: Feeling unusually tired even with minimal exertion.
- Chest Pain: Often described as pressure or tightness.
- Dizziness or Fainting (Syncope): Occurs due to insufficient blood flow.
- Palpitations: Feeling of irregular or racing heartbeats.
- Swelling (Edema): Particularly in the ankles, legs, or abdomen.
- Cyanosis: Bluish color of the lips or skin due to low oxygen levels.
Diagnosis of Pulmonary Hypertension:
- Physical Examination: A doctor may check for abnormal heart sounds, swelling in the legs, or signs of low oxygen levels.
- Echocardiogram: An ultrasound of the heart to evaluate the size and function of the right ventricle and estimate pulmonary artery pressure.
- Electrocardiogram (ECG): Measures the electrical activity of the heart and can detect strain on the right side of the heart.
- Chest X-ray or CT Scan: Helps identify lung abnormalities or enlarged heart chambers.
- Right Heart Catheterization: A specialized procedure that directly measures the pressure in the pulmonary arteries, confirming the diagnosis of PH.
- Pulmonary Function Tests: Evaluate lung function to identify underlying lung diseases contributing to PH.
- Blood Tests: Can detect markers of heart failure or other underlying conditions.
Treatment of Pulmonary Hypertension:
Medications:
- Endothelin Receptor Antagonists: Help relax blood vessels in the lungs and reduce blood pressure.
- Phosphodiesterase-5 Inhibitors (e.g., Sildenafil, Tadalafil): Improve blood flow to the lungs by dilating blood vessels.
- Prostacyclin Analogues: Dilate blood vessels and prevent clotting in the lungs.
- Calcium Channel Blockers: May be used in certain cases to relax the blood vessels.
- Anticoagulants (Blood Thinners): Used to prevent blood clots, especially in CTEPH.
- Diuretics: Help reduce fluid buildup in the body caused by heart failure.
Oxygen Therapy:
- Supplemental oxygen is used for patients with low oxygen levels to improve breathing and reduce the burden on the heart.
Lifestyle Modifications:
- Exercise: Light to moderate physical activity is encouraged, but under the supervision of a healthcare provider.
- Dietary Changes: Reducing salt intake to avoid fluid retention.
- Avoiding High Altitudes: To prevent exacerbation of symptoms in patients with PH.
Surgical Options:
- Pulmonary Endarterectomy (PEA): A surgical procedure to remove chronic blood clots in CTEPH patients.
- Balloon Pulmonary Angioplasty (BPA): A less invasive procedure to open narrowed arteries in CTEPH.
- Lung or Heart-Lung Transplant: In severe cases where other treatments are not effective, transplant may be considered.
Pulmonary Rehabilitation:
- A supervised exercise and education program designed to improve the overall quality of life in PH patients.
Prevention of Pulmonary Hypertension:
- Early Management of Underlying Conditions: Controlling diseases like heart disease, lung conditions, or sleep apnea can help prevent the development of PH.
- Avoiding Certain Medications or Toxins: Avoiding drugs or toxins known to increase the risk of PH (e.g., appetite suppressants, recreational drugs).
- Healthy Lifestyle: Maintaining a heart-healthy lifestyle with a balanced diet, regular exercise, and smoking cessation can lower the risk of PH.
- Regular Monitoring for High-Risk Individuals: Early screening for those with a family history or predisposing conditions.
Prognosis:
The prognosis for pulmonary hypertension varies depending on the type and cause. While there is no cure for most forms of PH, treatments can manage symptoms and slow disease progression. Early diagnosis and appropriate therapy are key to improving quality of life and outcomes. Some patients may eventually require more advanced treatments, such as lung transplantation, particularly if the disease progresses despite medical intervention.

